Originally published May 18, 2020
Legal Nomads began in 2008 as a travel site, and during the subsequent decade it morphed into a travel and food site as I lived around the world. Then, it shifted into a place to share the reckoning and grief that accompanied an abrupt life change. These days, it remains a place to share my thoughts on what’s going on around us, even if now we are all not able to explore the outside world. For now I wanted to talk about masks.
Specifically cloth masks.
Specifically the fact that many people are resisting wearing them.
I’ve been banging on about masks since I wrote my previous COVID-19 piece in mid-March, including via Instagram. But the subject is so important that I wanted to address masks in a standalone post.
I believe in individual liberty. But we should not use the concept of liberty as a pretext for acting selfishly toward society as a whole. Entitlement to freedom in a moral sense evaporates when the exercise of that freedom becomes harmful to others. By now, there is overwhelming scientific evidence that wearing masks in public dramatically lowers the risk of you spreading COVID-19 to others. And as I reiterate below, given that a large percentage of COVID-19 cases are asymptomatic, you may be infecting others without even knowing it.
Let’s get to it.
Table of Contents
notes, “It’s like stopping gushing water from a hose right at the source, by turning off the faucet, compared with the difficulty of trying to catch all the drops of water after we’ve pointed the hose up and they’ve flown everywhere.”
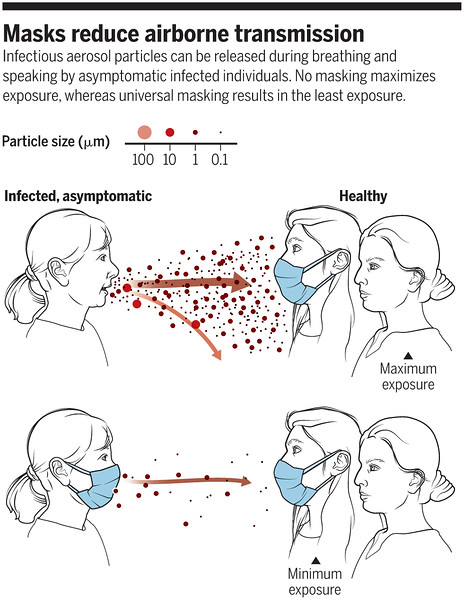
Here’s a graphic illustrating how stopping the droplets at the source helps curb spread of the virus:
Vol. 368, Issue 6498, pp. 1422-1424.
Infectious aerosol particles can be released during breathing and speaking by asymptomatic infected individuals. No masking maximizes exposure, whereas universal masking results in the least exposure.
Here’s a real-life depiction of the graphic above:
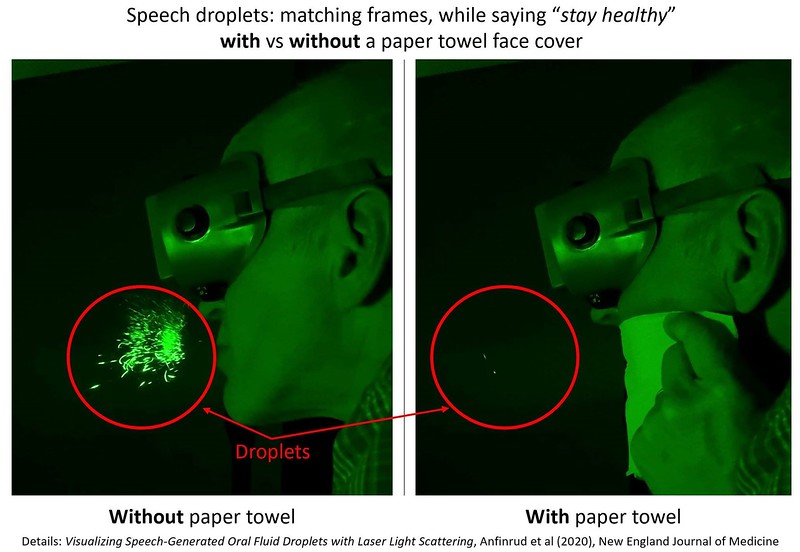
The two halves of the image above compare the emission of speech droplets by a researcher in a laser scattering chamber, with and without the speaker covering his face with a paper towel. As you see, nearly all of the outbound droplets are blocked. The reason speech was tested is that we now know it’s a common transmission mechanism for COVID-19 (via the upper respiratory tract), especially when the transmitter is not showing symptoms (i.e., not coughing or sneezing). The same principle by which a simple paper towel blocks outbound droplets applies when the speaker is wearing a mask.
When the pandemic was new, there was lots of focus on PPE for front-line medical workers in the press (and in studies), but little or no discussion in these sources about the benefit to everyone when the majority of society puts on a simple cloth mask. We wasted valuable time that could have prevented people from dying.
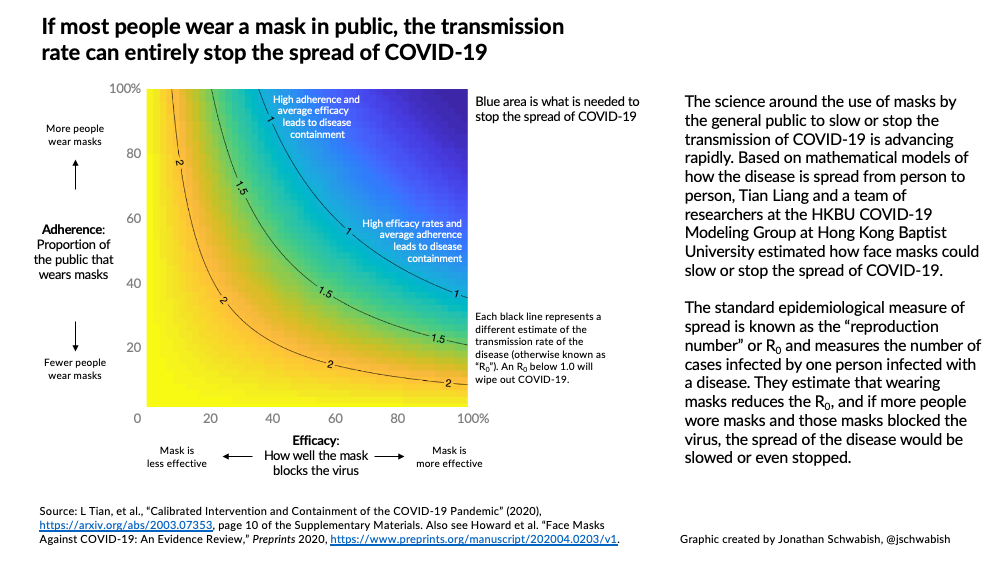
In countries where there was a swift about-face to require wearing of cloth masks, the transmission rates plummeted. A June 2020 study also confirmed that the countries that mandated mass masking earliest had the fewest deaths. “It wasn’t just by a few per cent,” said one of the study’s authors, “it was up to a hundred times less mortality. The countries that introduced masks from the very beginning of their outbreak have had hardly any deaths.”
And thankfully, more and more countries are following in their footsteps.
As a June 2020 study from the UK noted, “A key message from our analyses to aid the widespread adoption of facemasks would be: ‘my mask protects you, your mask protects me’.”
Using a mask can help lower the risk of your unknowing transmission of COVID-19 to others
COVID-19 can spread in different ways, and one of them is via the droplets that hurtle out of our mouths. In fact, a June 2020 study confirmed that airborne transmission is the dominant means of transmitting COVID-19, and that mitigation measures that do not include the mandatory wearing of face masks are insufficient to curb spread:
In this work, we show that airborne transmission, particularly via nascent aerosols from human atomization, is highly virulent and represents the dominant route for the transmission of this disease. However, the importance of airborne transmission has not been considered in establishment of mitigation measures by government authorities ([1, 20]. Specifically, while the WHO and the US Centers for Disease Control and Prevention (CDC) have emphasized the prevention of contact transmission, both WHO and CDC have largely ignored the importance of the airborne transmission route [1, 20]. The current mitigation measures, such as social distancing, quarantine, and isolation implemented in the United States, are insufficient by themselves in protecting the public. Our analysis reveals that the difference with and without mandated face covering represents the determinant in shaping the trends of the pandemic worldwide. We conclude that wearing of face masks in public corresponds to the most effective means to prevent interhuman transmission.
Ok, so COVID-19 is transmitted via outburst of droplets. How does this occur? It happens when cough or sneeze, but also when we speak. A single cough can release 3000 droplets. A portion of these droplets quickly evaporates to become something called droplet nuclei, which are tinier particles that are harder to protect against. They can be easily inhaled by anyone nearby.
But wearing a cloth mask has been shown to slow down that evaporation process. So much so, that in studies, a cotton mask reduced the quantity of virus particles emitted from mouths by as much as 99 percent. (2) This is because in the moist space between a person’s face and their cotton mask, it takes a lot longer for a droplet to evaporate into a droplet nuclei. The mask increases the humidity in that space, which prevents the droplets from getting tinier — meaning the fabric can still prevent them from being flung into the outer world.
Mass masking both prevents others from being infected by you, and if everyone is speaking moistly (3) into a mask, it lowers the overall burden of the virus in the area. Lowering the viral load in the area will also help protect essential workers.
People with no symptoms drive half of transmission for COVID-19
Here’s where COVID-19 throws a giant wrench into the common saying that you should only wear a mask if you’re sick: many people are transmitting this virus despite having no clue they are carriers. (4) This “oblivious transmission” issue is a huge driver of outbreaks for this pandemic. These oblivious carriers are divided into two categories: asymptomatic people, who never show symptoms, and pre-symptomatic carriers, people who are infectious but are not yet feeling any effects from carrying the virus – but will eventually develop symptoms.
As of mid-March 2020, studies were already showing that even if you’re fully asymptomatic, you can still spread this virus as a vector. Further articles demonstrated that the same is true for patients who will become symptomatic but are in a pre-symptomatic state. In fact, those patients are most contagious during the time when they’re pre-symptomatic.
A study from Japan released in June 2020 cited 61 clusters of COVID-19 outbreaks, each analyzed using contact tracing. The study found not only that many COVID-19 clusters were associated with people breathing heavily in close proximity to each other, such as singing at karaoke parties, cheering at clubs, having conversations in bars, and exercising in gymnasiums; but also that the most common age groups among those spreaders were 20–29 years (27%) and 30–39 years (23%) — and that an analysis of 16 of the clusters showed that 41% of the spreaders had no symptoms when they transmitted.
10) “For 16 clusters, we determined date of transmission and found 41% of probable primary case-patients were presymptomatic or asymptomatic at the time of transmission; only 1 had a cough at the time of transmission!”
➡️ MANY NO SYMPTOMS FOR INITIAL OUTBREAK EVENT! Masks now! pic.twitter.com/zAD7aELGje
— Eric Feigl-Ding (@DrEricDing) June 14, 2020
So if people only wear masks when they’re actually showing symptoms, that doesn’t fix the problem.
Wearing a mask does not mean social distancing and hand-washing are off the table
Have you seen people moving their masks around to talk? Or touching their faces and then food? Yes, me too, and it’s horrifying.
Mass masking is not a substitute for other precautions, and still requires the same amount of common sense as we needed to exercise pre-mask wearing. Social distancing and hand-washing are still critical to control the spread of COVID-19.
Just because you wear a mask doesn’t mean you should go and cuddle up to someone you haven’t seen in awhile. It doesn’t mean that you should ignore the social distancing recommendations. And as the weather warms up, it certainly doesn’t mean you head out and throw caution to the wind.
It means: add this one simple thing to your existing routine, and you will help save many lives.
And while the studies establishing that masks prevent transmission of COVID-19 are overwhelming, a recent real-world example demonstrated powerfully the difference that facial coverings make: In June 2020, the Springfield-Greene County Department of Health in Missouri reported that 2 hairstylists at a hair salon in the town of Springfield had serviced a total of 140 customers while infected with the SARS-CoV-2 virus in May. However, the hairstylists wore masks at all times during appointments. Not a single one of their 140 customers (or 6 co-workers who had potentially been exposed) contracted COVID-19. While other measures that the hair salon had in place (such as distancing of chairs and staggering of appointments) likely also played a role, it’s difficult to dispute that the wearing of masks by the infected hairstylists contributed heavily to preventing all of their customers and colleagues from contracting COVID-19. Indeed, Springfield-Greene County Director of Health Clay Goddard stated, “This is exciting news about the value of masking to prevent COVID-19.”
It’s as easy as that.
As a piece on masks in the Atlantic states,
[O]rdinary people are not helpless; in fact, we have more power than we realize. Along with keeping our distance whenever possible and maintaining good hygiene, all of us wearing just a cloth mask could help stop this pandemic in its tracks.
There is still some opposition to cloth mask wearing, so I wanted to address a few of the objections here:
1/ “Hypoxia (deprivation of oxygen)”. No, hypoxia is not an issue with breathable cloth masks.
In the video below, research scientist Jeremy Howard shows why wearing a cloth mask causes virtually no reduction in your inhalation of oxygen: most of the air that you’re breathing in comes from outside the mask.
This science is borne out by actual measurements of a mask wearer’s blood oxygen saturation level. Vlogger Tim from TheTimTracker, wore a tight, 2-layer fabric mask during a visit to some Disney properties in Florida for over 3 hours on a hot day; and he used a pulse oximeter to measure his oxygen saturation before, during, and at the end of his visit.
Per the Lung Health Institute, the normal range for a pulse oximeter reading for an adult is 94 to 99%, while a level below 90% is cause for concern. Prior to donning his mask, Tim’s oxygen saturation level according to his pulse oximeter ranged between 96 and 97%. While he was masked and doing a great deal of walking around in the heat, his pulse oximeter readings remained between 95 and 97%; and at the end of his visit to the Disney venues, his reading was 96%.
Since Tim’s video is long, if you want to view the portions where he measures his oxygen saturation level, you can find them beginning at 1:32 (initial, pre-mask reading); 10:16; 15:12; 17:41; and 23:37. The video confirms that your intake of oxygen isn’t meaningfully decreased when you wear a cloth mask.
Yes, it’s hard for doctors to breathe in N95s, and I empathize with their needs to wear PPE (masks and gowns and more) for long stretches since that equipment is very uncomfortable, but that’s the only way for them to be safe in treating people who come in with COVID-19 given the high viral loads they are exposed to at work. In contrast, as shown above, cloth masks that you and I can wear don’t cause comparable difficulties in breathing.
And even for those with asthma, wearing masks is recommended.
2/ “Ok fine no hypoxia. Hypercapnia (abnormally elevated carbon dioxide (CO2) levels in the blood)”. Also a no. Arguments that wearing a mask can do this due to “rebreathing your own exhaled CO2 by wearing a mask continually” are false. Many doctors, scientists, and industrial workers have routinely worn masks for prolonged periods of time without any clear adverse effects. As this AP piece fact-checking the hypercapnia claim states, “with how common mask wearing has always been, even before COVID-19, we would know if hypercapnia was a problem with wearing masks.” In addition, since I’m advocating for wearing masks made from breathable cotton, the hypercapnia claim is even more baseless than if I were urging everyone to don an N95.
3/ “Studies about the size of the droplets for COVID-19 show that they’re small microns, so cloth masks don’t work.” Yes, that’s the big issue with ingress: inbound droplets. But my argument for cloth masks is based on egress, outbound droplets. The studies cited below are specifically using conditions comparable to COVID-19, and are new because we didn’t focus too much on egress previously – but now we have great reason to. We are trying to prevent giving others our droplets, and that’s why cloth masks only work if we all wear them. We’re trying to make sure we don’t unknowingly contaminate others.
4/ “I can just stay further away from someone when I go out and not wear a mask.” The experts have weighed in on this one, and explained that merely keeping your distance from others without wearing a mask isn’t safe enough. Droplets emitted when there’s no mask to block them scatter into a cloud, and they then hang around in the air for about 10 minutes. See research scientist Jeremy Howard’s tweet below, which addresses this issue. So even if you’re not immediately next to anyone when you breathe out droplets, a person who wanders into the area several minutes later can still be exposed.
I’ll post additional tweets to answer questions here. First question in the replies was: Is it enough to just avoid getting in front of people?
No. Droplets hang around for 10 minutes or more, and can blow around into a cloud formation.https://t.co/SIpZjtVHkN pic.twitter.com/tZYEX5rzAg
— Jeremy Howard (@jeremyphoward) June 19, 2020
5/ “I tried wearing a mask but my glasses fog up when I do.” Yes, the fog is real. I am nearsighted and have experienced this issue. It’s true that when you wear eyeglasses, your warm breath exhaled through the top of your mask can fog up the lenses of your glasses. Fortunately, there are workarounds. A full discussion of ways to prevent the fogging-up problem, provided by the Cleveland Clinic, here. Additional tips via the Pittsburgh Post-Gazette here. Among the anti-fogging techniques: (a) washing the lenses of your glasses with soap and water; (b) putting a folded tissue under your mask at the top, to absorb the moisture so that it does not fog up your glasses, or (c) using anti-fog sprays designed to defog glasses. There are many solutions to choose from that enable you to wear a mask while still seeing clearly. I prefer the soap and water technique in the video below, but if you want anti-fog sprays, here’s a round up of the best ones.
Also, for those who don’t want to add the tissue yourselves, MasQuebec sells a mask with the added piece of material built in, specifically for people who wear glasses, which you can find here.
VIDEO: How to wear a mask without your glasses fogging up. The second technique is the one that works for me.
6/ “But doctors need masks” Yes, that’s why we aren’t using theirs. The piece you are reading (and others, see the sources below) discuss how cloth masks work very well to stop the spread of COVID-19 if worn by the vast majority of people when out in public.
7/ “But the CDC said not to wear them if healthy” Reality is that this is a new virus and scientists and doctors are all learning as they go. Once epidemiologists and other medical professionals realized the staggering percentage of cases transmitted via asymptomatic vectors, they – including the CDC – shifted from their initial guidance to now recommend the wearing of cloth masks. And countries such as the Czech Republic and Austria that switched course quickly to mandate masks are faring a lot better than those that did not.
8/ “Masks increase the risk of infection for the wearer.” Back in March 2020, which is basically decades ago in COVID-19 time, the U.S. Surgeon General and others were recommending no wearing of masks, and opined that wearing certain types of masks increased the risk of infection for the wearer. At that point in time, the discussion was about N95s and surgical masks, and those same articles discussed ensuring adequate PPE supply for doctors, nurses, and other healthcare workers. Here we are talking about a cloth mask, which is a very different situation as purchasing or creating a DIY one does not imperil the supply of medical masks for the medical professionals who need them. And again this is a discussion about egress, not ingress. There was a 2015 study from Hanoi, Vietnam about how cloth masks worn by healthcare workers who are in close contact with sick patients for long periods of time increased those healthcare workers’ risk of respiratory infection. That is again not what we are talking about here. You and I are not healthcare workers who are going to wear our masks while attending to hospitalized patients; our mask wearing as stated above is about not infecting others.
9/ “But freedom!” I know some people have been convinced that freedom is at stake, but if we look around the world the countries that did mandate mask wearing – or had cultures of most members of their populations voluntarily wearing masks in public (which in the latter case were East Asian countries where people had memories of the SARS and H1N1 influenza pandemics that hit that region hard) – are those that tend to be doing the best. Many never even felt compelled to impose lockdowns because the virus never spread in an uncontrolled fashion within their borders; and those that did are now opening up. Their people are now able to move around safely. In contrast, in many of the countries whose citizens have not worn masks in large numbers either voluntarily or under government mandate, the virus is still spreading rapidly.
After living in Asia for many years, where it’s considered customary and reasonable to protect others from becoming infected by you when you’re ill, I wore masks when unwell with contagious diseases. Excluding specific and limited exemptions, for example people who are hearing-impaired* or have a disability that makes it hard for them to wear or remove a face covering, there are only self-focused reasons not to wear one during a pandemic. And this is not a time to be self-focused.
I wear a cloth mask to protect others, but that can only have a meaningful impact in reducing the society-wide harms from COVID-19 if others do the same.
The freedom to breathe on others in ways that may kill them is just not a reasonable thing to desire.
-Jodi
* There are ClearMasks for the hearing-impaired community, but to my knowledge they are not widely available nor widely accessible.
***
Where to Buy Cloth Masks
I got mine from my friends Bethany and Randy, who are sewing them and donating one for every one sold. You can get yours here. They are also making them with pockets so that filters can be added if desired. Be sure to specify in the notes section if you have a particularly small or large face.
Options for cloth masks for kids, to be put on and removed with parental supervision, can be found here.
Another option is to make masks at home, if you’re able to. Patterns abound.
- Pleated surgical-style mask out of fabric, here.
- Craft Passion’s mask with covering for the nose and elastics around the sides here, in 4 different sizes including for kids ages 2 and up.
- Masks for the hearing-impaired here.
Cloth masks should fit snugly but comfortably, and be tied with elastics or adjustable fabric. They ought to contain at least two layers of breathable fabric, and be able to be washed (see below) without damaging the materials.
Good Housekeeping notes that “tightly woven, 100% cotton is the best fabric to use, which means you can turn a bandana, or fabric from pillowcases, curtains, or woven shirts into a face mask or covering. Be sure to avoid knit fabrics, like jersey T-shirts, because they create holes when stretched. To make the mask even more protective, use a nonwoven interface, coffee filter, or HVAC filter (as long as they don’t contain fibreglass) inside the mask to help block particles.”
Proper Care for Cloth Face Masks
Yes, these masks need to be washed and cared for in order for them to keep working. I launder mine in a washing machine on a gentle cycle, or hand wash them with hot, soapy water, after each use.
As with anything you may touch that may be contaminated, it is important to wash your hands if you have touched your face with your mask on (or if you touched the mask itself while wearing it), so that you don’t contaminate the next thing you touch. Also, after removing your mask (which you should do only by handling the straps or other piece that secures it, and never by grabbing the front of the mask), thoroughly wash your hands for those 20 seconds you now know well.
Sources
(1) On droplet size
(2) On how cotton masks can help curb the spread of COVID-19
(3) The “speaking moistly” is a reference to Canada’s PM Justin Trudeau, who used the phrase at a press briefing — and seemed to immediately regret it.
Someone creative made it into an autotune song, and it is glorious:
(4) On asymptomatic and pre-symptomatic carriers:





